Breast Reconstruction Surgeries
Breast Reconstruction
Breast reconstruction is the surgical creation of a breast using either a synthetic implant or tissue from another part of your body. The aim of breast reconstruction is to create a symmetrical breast which is soft, natural and closely resembles your normal breast.

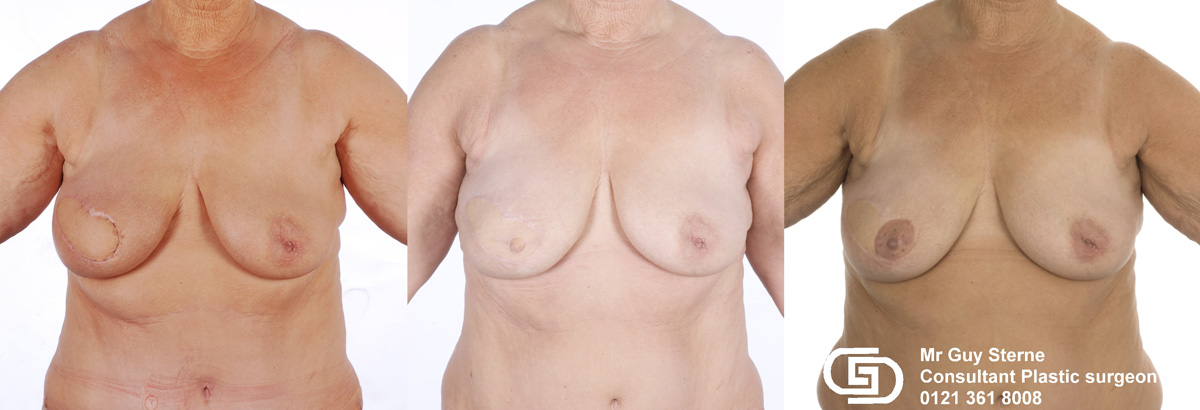
Delayed left breast reconstruction with a Latissimus Dorsi flap. The picture on the left demonstrates a typical mastectomy scar. The photo on the right shows the reconstructed breast together with a reconstructed nipple and tattooed areola[/caption]
A breast reconstruction should be considered by any woman who requires a mastectomy. Some patients may decide that they do not wish to undergo breast reconstruction and have a simple mastectomy instead. There are a number of issues which need to be considered when considering a breast reconstruction. These decisions can be quite difficult and should be talked through with your breast cancer surgeon. If your breast cancer surgeon does not perform breast reconstruction themselves you will also be referred to a plastic surgeon who specialises in this area.
The aim of the following pages is to help you with this decision by providing you with information which should be considered before making your decision. The final decision is yours, but can only be made in conjunction with your surgeon/medical team.
There are 4 groups of patients who may consider a breast reconstruction:
- Newly diagnosed breast cancer
- Previous mastectomy
- High risk of developing breast cancer
- Previous breast cancer treatment which has deformed the breast
There are several surgical options for treating a newly diagnosed breast cancer. These will be discussed with you by your breast cancer surgeon.
- Wide Local Excision and Radiotherapy: The tumour and a small amount of surrounding breast tissue is simply removed from the breast. This is a good decision for women with small tumours. Removal of a small amount of tissue from the breast causes little deformity and little change in size. The scarring is minimal, the breast remains soft and sensate (ie it feels normal). However, the remaining breast tissue must receive radiotherapy to reduce the risk of local recurrence.
- Therapeutic Mammaplasty and Radiotherapy: The breast cancer can be removed from the breast with a larger margin of normal breast tissue (ensuring safe removal) and the remaining breast tissue can be reshaped to make a smaller, perter breast. This is a good option for women with larger cancers in larger breasts, and for those who would benefit from having their breasts made smaller. The opposite breast can be reduced to result in two symmetrical, smaller breasts. As with a Wide Local Excision, the remaining breast tissue must receive radiotherapy to reduce the risk of local recurrence.
- Mastectomy: This is usually recommended for larger tumours in smaller breasts or when there are two or more tumours in the breast. All of the breast tissue is removed. This has the lowest risk of breast cancer returning. Subsequent radiotherapy is only needed for certain tumour types. When a mastectomy is being considered, the option of breast reconstruction should always be discussed, together with the timing of any proposed breast reconstruction.
A breast can be reconstructed at three distinct times related to the mastectomy surgery:
Immediate Reconstruction
If a breast is reconstructed at the same operation as the mastectomy, it is known as an immediate breast reconstruction. Immediate breast reconstruction has been shown to be safe. It does not increase the risk of the cancer coming back and it does not prevent the detection of a cancer if it does come back. Immediate breast reconstruction has certain significant advantages:
- Psychological Benefit: You wake up with a breast and never experience a mastectomy defect. The psychological benefits are obvious.
- Fewer Operations: Because the two operations are done together
- Cosmetic: The skin of the breast can be kept, meaning that there is less scarring, a better breast shape and a better overall cosmetic outcome
However, immediate breast reconstruction also has some definite disadvantages:
- Less time to make decision: Usually an immediate reconstruction is done following a diagnosis of breast cancer. In this case there is an urgent need to proceed with cancer removal. This leaves very little time to decide on breast reconstruction.
- More complications: Because a combination of mastectomy and breast reconstruction together carries more chance of complications than a mastectomy alone. Also, there is less time to optimise patient health (eg stop smoking, lose weight, control other medical problems) which increases the risk of complications too.
- Possible delay in chemotherapy: Depending upon the type of breast cancer, some patients will require chemotherapy after their mastectomy. This chemotherapy is most effective if it is given within 6 weeks of the mastectomy. However, chemotherapy can only be given once the surgical wounds have fully healed. Wound healing complications are more likely after immediate breast reconstruction.
- Postoperative radiotherapy may damage the reconstruction: Depending upon the type of breast cancer, some patients will require radiotherapy after their mastectomy. This radiotherapy will quite likely damage the breast reconstruction.
Delayed Reconstruction
If the breast is removed first (mastectomy) and the breast is reconstructed after a period of months or even years, this is known as a delayed breast reconstruction. Delayed reconstruction can sometimes be the better option. It would be recommended for women:
- Who have certain cancer types: There are some types of breast cancer where it is not wise to do an immediate breast reconstruction because of the high risk of the cancer coming back. In these cases it is usually better to proceed with a mastectomy, and then complete post-mastectomy chemotherapy and radiotherapy before considering a delayed breast reconstruction. Your breast cancer surgeon will advise you on this.
- Who are more likely to experience complications: ...for example heavy smokers, the significantly obese, or those with other medical problems which increases the risk of complications too.
- Who do not wish to risk possible delay in chemotherapy: Depending upon the type of breast cancer, some patients will require chemotherapy after their mastectomy. This chemotherapy is most effective if it is given within 6 weeks of the mastectomy. However, chemotherapy can only be given once the surgical wounds have fully healed. Wound healing complications are more likely after immediate breast reconstruction.
- Who will definitely require postoperative radiotherapy: Because this radiotherapy will quite likely damage the breast reconstruction, it may be better to proceed with a simple mastectomy, then receive radiotherapy and then, six months after the radiotherapy has been completed, a delayed breast reconstruction can be performed.
Prioritizing
Being advised against an immediate breast reconstruction can sometimes be disappointing, but in all cases the cancer treatment must take priority over the cosmetic outcome. None of the above recommendations are absolute and you should discuss your wishes and motivations with your surgical team.
Delayed-Immediate Reconstruction
This is a newer, less commonly used procedure. It is useful for fit, healthy, younger women with a high cosmetic demand who have been advised to proceed with a mastectomy alone and are planning a delayed breast reconstruction. The quality of the cosmetic outcome depends upon the breast skin. If the breast skin can be preserved, then the cosmetic outcome is usually better because it avoids the ?patch? of skin that is seen with the delayed reconstruction. It is not possible to remove the breast tissue and simply leave the breast skin because the empty skin will scar up, shrink and develop deep wrinkles. It is not possible to eradicate these wrinkles later. However, the breast skin can be ?banked? by inserting a tissue expander into it to stop it from shrinking and wrinkling up. Then later, the tissue expander can be removed and the breast can be reconstructed using living tissue from another part of your body. This preserves the breast skin, minimises scarring and therefore has the same cosmetic advantage as an immediate reconstruction.
There is however a disadvantage to this approach. Having a tissue expander under the skin increases the risk of the breast skin breaking down after the mastectomy. If this happens, any planned chemotherapy would be delayed, which reduces the effect of the chemotherapy.

This is the simplest method of breast reconstruction and reproduces the skin envelope by stretching the remaining skin and muscle of the chest wall. This is done in 2 short operations about 8 -12 weeks apart. In the first operation, under general anaesthetic, the old mastectomy scar is opened and a tissue expander placed beneath the skin and muscle.
A tissue expander consists of an inflatable silicone bag with an inflation port attached via a tube. The expander is inflated by injecting saline through skin into the port, which stretches the overlying skin. This stretched skin becomes tight but not painful. Over the following few days the skin relaxes allowing a further expansion the following week. Serial inflation commences in the outpatient department about two weeks postoperatively and continues on a weekly basis until the skin has been sufficiently stretched - usually by eight to twelve weeks. Most patients continue working during this period of expander inflation.
Once the inflation process is completed and a sufficiently large skin envelope has been created, a second operation is performed under general anaesthetic. The saline filled expander is removed and replaced with a silicone implant which produces a more natural feel and appearance than the saline filled bag.
Each operation takes about one hour, the patient stays in hospital for one or two days and usually recovers by two weeks.
Although a two-stage procedure has been described, newer tissue expanders are now available which consist of a tissue expander inside a silicone implant. This device can be used to expand the skin creating a skin envelope but as it contains silicone too it also feels like breast tissue and therefore does not need exchanging for a silicone implant - thus avoiding a second operation.
Advantages and disadvantages
- Simplest method of breast reconstruction
- Reasonable shape:
- Good volume match possible with small and medium sized breasts
- Very little additional scarring to the breast.
Its main disadvantages are that it requires:
- Multiple outpatient visits for expansion,
- Two separate operations: although with the newer implant/expanders this second operation can be avoided
- Has a higher complication rate due to the foreign nature of the prosthesis.
- Not usually advised for patients with marked radiotherapy damage or for patients with poor condition skin of the chest wall.
Possible complications
- Exposure of the Expander: The overlying skin thins to some extent with tissue expansion, occasionally the skin may thin so much the expander becomes exposed and subsequently infected. This may result in failure and may lead to an alternative method of breast reconstruction.
- Infection: This is the commonest complication of tissue expansion, it may be managed with antibiotics and rest but occasionally it results in failure of the operation and requires removal of the tissue expander. In this event, several months later once the infection has completely settled tissue expansion can be reattempted. The infection rate following the second operation is about 3% and whilst some settle with antibiotics, others require surgical removal of the implant, which can then be replaced several months later once the infection has completely settled.
- Capsule Formation: Insertion of any foreign material into the human body results in the body forming a wall of scar, known as a capsule, around that material. In about 10-15% of patients with a silicone implant, this capsule contracts around the prosthesis resulting in a painful, hard, distorted breast. Severe capsular contracture requires surgical treatment and, occasionally, removal of the silicone breast prosthesis.
- Slow Leak or Rupture: Is an infrequent event occurring in 0.5 - 5% of cases and usually results from direct, substantial trauma to the breast. Minor blows to the breast and flying at altitude are insufficient to rupture a silicone breast prosthesis and are perfectly safe. Although silicone leakage can sometimes causes swelling of the lymph nodes in the arm pit, in the majority of cases it causes no problems.
- Permanence: It is not known how permanent the new generation of silicone breast implants is, but the manufacturers suggest the implants may require changing after 10-15 years.
 This patient underwent a left mastectomy and immediate, simultaneous breast reconstruction with an ELD flap and she also received a small breast implant in the right breast.
This patient underwent a left mastectomy and immediate, simultaneous breast reconstruction with an ELD flap and she also received a small breast implant in the right breast.
Lattissimus Doris and Breast Reconstruction
The latissimus dorsi is a large muscle found on the back which acts to pull the arm into the side and backwards. This muscle, together with a large piece of skin and fat overlying it, can be moved to the front of the chest. It is kept alive by maintaining its blood vessels intact. The skin and muscle are then tunnelled under the skin around the chest wall and into the breast pocket to create the new breast. If the opposite breast is quite large and there is insufficient tissue available on the back to match this volume, it is possible to include a breast implant beneath this flap to create a larger breast, however, if the patients choice is to avoid using an implant, the breasts can be made an equal size by reducing the size of the normal breast. It is also possible to tailor the scar on the back; the scar can be horizontally orientated to be hidden beneath the bra straps or can be obliquely orientated so that it is not visible beneath strapless or backless garments. This should be discussed with your surgeon.
The procedure is performed under a general anaesthetic and several drains are required postoperatively in the back and the newly reconstructed breast.
As a rough guide the operation takes about 4 hours, needs 4 days in hospital and takes about 4 weeks to recover.
In general, despite the latissimus dorsi being a large muscle, its transfer does not result in any noticeable functional deficits, as there are other, smaller muscles around the shoulder which do the same job.
This flap is almost always available for use, though occasionally the blood vessels supplying the latissimus dorsi muscle may have been damaged at the original mastectomy. Breast surgeons are very aware of the possible future need for breast reconstruction with this flap and attempt to preserve this vessel if at all possible.
Use of the Lattissimus dorsi flap does have some advantages and disadvantages
Advantages:
- Simple: This procedure provides the simplest method of recreating a breast using living tissue. The single stage operation is much quicker and is far better tolerated by the patient than a TRAM flap.
- Avoids Silicone Implant: When used alone it is free from the complications associated with a silicon prosthesis.
- Postoperative Recovery: Recovery period is fairly short and the flap is very reliable and safe, because it remains attached to its original blood supply.
Disadvantages:
- Reconstructing Moderate Size or Large Breasts: It is difficult to reconstruct a moderate sized or large breast due to the limited tissue available, though this may be overcome by either including a silicone prosthesis or tissue expander beneath the flap or by reducing the size of the normal breast.
- Donor Site Scarring: The donor site scar on the back is more obvious than that of the TRAM flap, and produces characteristic hollowing on one side when viewed from behind.
- Patch of Pale Skin: The skin from the back is thicker and paler than skin on the chest, resulting in an obvious patch of pale skin within the new breast.
- Creating Symmetry: There is a higher incidence of operations on the normal breast to achieve symmetry.
Possible Complications
Generally latissimus dorsi breast reconstruction is a safe, reliable technique with few potential complications
- Flap Failure: Because the flap is never detached from its blood supply it is very rare, less than 1%, for this flap to fail
- Partial Flap Failure: In heavy smokers or patients with known circulatory disease, part of the flap may die resulting in scarring and a slightly smaller breast than desired.
- Seroma: Despite the use of drains, it was quite common for fluid to collect beneath the scar on the patient's back which could cause swelling and discomfort. More recent techniques have significantly reduced this complication and it is now seen very infrequently.
TRAM or DIEP Flap Procedure
 This patient underwent a right mastectomy and her breast was immediately reconstructed with a pedicled TRAM flap.
This patient underwent a right mastectomy and her breast was immediately reconstructed with a pedicled TRAM flap.
In a TRAM or DIEP flap breast reconstruction skin, fat and muscle is taken from the lower abdominal wall and used to recreate the breast. This abdominal tissue is kept alive in one of two ways depending upon surgical preference.
1. The tissue can be kept connected to its blood supply and tunnelled into the breast. This is called a pedicled TRAM flap. Or alternatively...
2. The tissue can be completely removed, repositioned on the chest wall and its blood vessels reconnected to an artery and vein in the armpit or chest using microsurgery. This is called either a free TRAM flap or a DIEP flap.
In each case, the resulting wound in the abdominal wall is closed producing a similar effect to a tummy tuck.
The procedure is carried out under a general anaesthetic and several drains are required in both the abdomen and the newly reconstructed breast. A catheter is usually placed in the bladder for 48 hours for patient comfort. Following the operation the patient is kept on bed rest and nursed in a very warm room for several days to encourage blood flow into the flap.
Postoperative pain is highly variable but in general the abdominal part of the operation is the more uncomfortable. Pain relief is usually given in the form of morphine for the first 48 hours, followed by strong painkilling tablets.
As a rough guide a TRAM flap breast reconstruction takes about 7 hours, requires 7 days in hospital and takes 7 weeks to recover from. The abdomen takes 7 months to regain near normal suppleness.
Advantages, Disadvantages and Possible Complications
Advantages
- The tram flap provides a new breast of soft, warm, living tissue which will put on or lose weight with the rest of the patient and has the most natural appearance of all the breast reconstruction methods.
- It enables a large breast to be reconstructed in a single operation
- Avoids the disadvantages of a silicone prosthesis.
- Additional advantage of a flatter abdomen.
Disadvantages
- This reconstruction is a far bigger procedure than the original mastectomy and will be correspondingly more stressful. However, the benefits in terms of the new breast help to alleviate this.
- Low mid-line abdominal scars may prevent the use of the TRAM flap due to damage to local blood vessels, which supply tissue required for transfer.
Possible Complications
- Infection
- Bleeding
- Wound Healing Problems: This is seen particularly in patients who smoke
- Flap Loss: One in 10 flaps undergoing a micro-surgical connection will develop some problem with the blood supply within 48 hours of surgery. These need to return to theatre in an attempt to restore the blood supply. One in twenty flaps fail completely.
- Partial Flap Loss: This problem is mostly seen with those flaps which remain connected to their original blood supply and are tunneled into the new breast. It occurs in X% flaps.
- Fat Necrosis: This can occurs in about 5% of cases as a result of inadequate blood supply to part of the flap. This results in the death of a portion of tissue which initially swells becoming painful and hard and eventually shrinks forming a hard scar within the breast.
- Abdominal Hernia: The removal of part of the muscle of the abdominal wall results in some weakness there and an increased risk of bulging or hernias. This complication is seen about 5% of cases
- Dog-Ears: Occasionally there will be small folds in the skin and fat at either end of the abdominal scar known as dog-ears which may require surgical excision or liposuction under local anaesthetic at a later date.
Breast Cancer - Risk Management
The lifetime risk of any woman developing breast cancer is currently estimated to be 1 in 8. The vast majority of these breast cancers occur in much older women. Some younger women, because of genetic factors, have a much higher risk of developing breast cancer. This high risk group can be managed in 2 ways:
1. Screening: In which they can either undergo yearly xrays or MRI to identify any worrying signs early.
2. Risk Reducing Mastectomy: In which they can have both breasts removed before any cancer develops. The aim of this operation is to remove as much breast tissue as possible in order to reduce the chance of the breast tissue turning into breast cancer. A mastectomy cannot remove 100% of the breast tissue, and as such, there will always be a small chance of developing cancer afterwards. However, a risk reducing mastectomy does massively (90-95%) reduce the risk of developing cancer.
What if breast cancer is in my family?
If a woman has a strong family history of breast cancer then they should discuss this with their family doctor who will probably refer them to their local breast cancer unit. Here, a full team of specialists will be available to help with advice. A geneticist will be able to estimate the lifetime risk of developing breast cancer and may also offer gene testing (a simple blood test). If the patient is thought to be at high risk, then a breast surgeon will discuss the options of regular xrays or surgery. If the patient wishes to proceed with surgery, then a clinical psychologist will help the patient talk their decision through and a plastic surgeon will discuss the reconstructive options.
Pre-Operation Considerations
Once a decision has been made to undergo a risk reducing mastectomy there are several things to consider:
Do I want a reconstruction? Not everyone wishes to undergo a breast reconstruction - some women just want to have their breasts removed to reduce the risk of getting breast cancer. Most women however do want breast reconstruction.
What will the results of reconstruction be like? It is important to realise that the newly reconstructed breasts will not be normal breasts. They will feel somewhat numb, and are usually a little firmer than normal breasts. There will be no erogeneous sensation in the nipples and of course, breast feeding will not be possible. However most women are delighted with the outcome of surgery and are confident that they made the right decision.
What reconstruction should I have? The key choice here is whether you want an implant-based reconstruction or a living tissue reconstruction. A living tissue reconstruction gives the best cosmetic outcome, and produces soft, natural looking breasts which usually last a lifetime; however, this is a big operation, takes a long time to recover from and results in a donor site scar and possible donor site complications. An implant based reconstruction is a smaller, safer, simpler operation which does not require a donor site. Recovery is generally faster which makes this a popular reconstruction option for younger women who have a young family. The final outcome is not usually quite as good, but because both breasts are being replaced the outcome will be symmetrical and the breasts will behave similarly over time. The disadvantage with implant based reconstruction is that the implants may not last forever and may need further operations at some stage in the future.
What should I do with the nipples? The aim of the risk reducing mastectomy is to remove as much breast tissue as possible in order to maximally reduce the risk of developing breast cancer. A small amount of breast tissue is present within the nipples. Removing the nipple therefore maximally reduces the risk of cancer. However, it is difficult to reconstruct a realistic nipple and many surgeons advocate keeping the nipple. This results in a cosmetic advantage and only very slightly increases the risk of developing a cancer (about 1% more). Furthermore, if any cancer does occur, it would present as a lump in the nipple, which would be easy to feel and detect.
When should I have risk reducing mastectomy? This is a personal choice and depends upon individual circumstances. Factors to consider include; the average age when family members developed breast cancer; whether or not you plan to have children; are you as fit as you could be.
Some gene abnormalities (e.g BRCA2) also increase the risk of developing ovarian cancer and this risk is often managed by removing the ovaries. There has been much discussion about whether this could be done at the same time as a risk reducing mastectomy. Personally, I advise against this combined surgery as the potential complications of one operation may jeopardise the outcome of the other.
- Implants - dermofascial flap
- Strattice
- Two stage reconstruction with tissue expander, then implant
- Living tissue ELD
- TRAM/DIEP/FREE TRAM
- SGAP/IGAP/TUG
The commonest surgical treatment for breast cancer is a Wide Local Exicision (lumpectomy) followed by radiotherapy. The advantages of this approach are that the breast is preserved and it usually results in minimal scarring and has little or no effect on the shape of the breast. Unfortunately however, it sometimes leads to deformity of the breast, or shrinkage of the breast resulting in breast asymmetry. If the deformed breast has previously been irradiated, then it is not usually possible to use an implant and any surgery to the irradiated breast (other than doing a mini-flap from non-irradiated tissue) usually results in wound healing problems. Despite this limitation, there are a number of options available for dealing with these deformities:
- Fat grafting
- Mini-flap to restore the shape
- Reduce and reshape the opposite breast
- Remove the whole breast and start again
The ideal goal of breast reconstruction is to produce a perfect match, in terms of size and shape, with the opposite breast. However, this is not always possible with reconstruction alone and about one third of all breast reconstruction patients may be offered some surgical procedure to their normal breast to achieve a reasonably good match. Matching operations to the normal breast include
- Breast enlargement
- Breast reduction
- Breast uplift
- Risk reducing mastectomy
- Using skin reduction
- Liposuction
- Fat grafting
- Get fit
- stop smoking etc
Use from my collection:
- implant based reconstruction
- Strattice
- Tissue expander
- ELD
- TRAM
- BREAST REDUCTION
- BREAST AUGMENTATION
- MASTOPEXY
- liposuction
- NIPPLE RECONSTRUCTION
- FAT GRAFTING
- LIPOSUCTION
- AREOLAR TATTOOING
The Butterflies Breast Reconstruction Support Group was founded in 2004. It was the first group of its kind in the country and gained Charitable Status in 2006. Its aim is to provide support to women considering breast reconstruction.
Support comes in many forms including formal talks, group evenings and networking. However, most people seem to prefer individual chats either over the phone or better still over a cup of tea. Butterflies has a large group of ladies, who have had a wide range of breast reconstructions and they try to introduce new patients to previous patients who underwent the same procedure. Talking to other women who have been through the same experience, is a great way to help inform and empower ladies contemplating breast reconstruction, and removes some of the mystery and fear of surgery.
It aims to provide patients with the maximum amount of information and support prior to their decision to proceed, and also during and after treatment.
Not only has Butterflies got access to ladies who have been through surgery and are happy to share their experiences and advice with the group, they also have access to a number of highly experienced professionals, and all Butterflies core members have been trained by McMillan Cancer Support.
Butterflies predominantly supports ladies from Birmingham, Bromsgrove, Kidderminster, Worcester and Walsall but regularly receives requests for help for ladies beyond the Midlands.
Further information is available on their website
info@butterflies-support.org.uk.
"...The day I was diagnosed with breast cancer was the most scary day of my life and I had no idea that I could feel good about myself and my body again. Once I met you, your energy and enthusiasm made me feel that I wanted to go ahead with reconstruction and that you would not let me down. I have no regrets at all and am so proud of my new breasts that I am afraid that I do wear more low cut tops than I did before!
We are so lucky in Birmingham that we have you and your team to help women overcome the horror of mastectomy. So once again, thank you from the bottom of my heart..." Mrs P.W., Birmingham: TRAM Flap Breast Reconstruction
"...How can I thank you enough, you have given me back myself... I feel like I have come full circle in my journey through breast cancer. My treatment with you Mr Sterne was second to none. I was treated with great kindness, compassion and respect. Words just do not come close to even begin to describe how I feel you have put me together again..." Mrs M.B., Birmingham: TRAM Flap Breast Reconstruction
"...Thank you so much for all your help patience and foremost your amazing skill at transforming my bust. It has been a long road for me and I know I haven...t been the most patient of patients, however I feel I have now reached the crossroads and I am so delighted with the result you have given me. I have now gone from despair and frustration to delight and determination and I am so looking forward to a new future with my wonderful new body..." Mrs J.C., Great Barr: Breast Reconstruction
"...I want to send you my very grateful thanks for all of your wonderful treatment during the last 4 years, from both you and also your team. I am very pleased with both my breast reconstruction and my reduction operation on the left breast. I have no regrets at all, and gladly pass on my views to other ladies considering such treatment..." Mrs A.G., Wolverhampton: Beast Reconstruction
"...I can't begin to explain what a difference the ...op... has made to my life. The result is far better than I had dreamed possible..." Mrs J.K., Telford: Latissimus Dorsi Breast Reconstruction
"...I am unable to express how I feel about what you have done for me. I am truly amazed at how you have been able to give me back (and a bit more) what means so much to any woman. I am so pleased with how I look; it has made such a difference to me; I thought, when I had my original surgery that it didn't matter. I was just so pleased that someone could remove the breast and save my life. I now realise that it really did matter. An awful lot. Once again, thank you so much. I will be forever in your debt, but forever singing your praises." Mrs S.T., Bromsgrove: Breast Reconstruction
"...How do I thank you for turning my life around..." Mrs L.H., Solihull: Breast Reconstruction
"...I know I gave you a bit of a hard time with an abdominal wound which refused to heal, following a double mastectomy and TRAM flap reconstruction, but we got there in the end didn't we... Life is back to normal now and hectic as ever, but I thought I would drop you a line to thank you and your team for the care I received. You really do have a gift for making people feel at ease in traumatic situations which goes far beyond any medical expertise, thanks for that. Being diagnosed with the BRCA1 gene was traumatic at the time, but the support I received from your team and Butterflies was fantastic and the results are great. If I can be of any help to you or the 'Butterflies Breast Reconstruction Support Group' in the future I would be more than happy to help..." Miss K.W., Great Barr, Birmingham: Bilateral Breast Reconstruction
"... Thank you for all your care and consideration AND your magnificent work." Mrs S.K., Bewdley: Breast Reconstruction